Cumulative prostatitis is accompanied by increased urination, dull pain in the lower abdomen and perineum, erectile dysfunction, presence of blood in the seminal fluid and prostatorrhea. Cumulative prostatitis can be diagnosed using a digital prostate exam, ultrasound of the prostate gland, urography and laboratory testing. Conservative treatment for suffocating prostatitis is carried out with the help of drugs, herbal medicine and physiotherapy. If these measures are ineffective, stone destruction with low intensity laser or surgical removal is indicated.
General information
Cumulative prostatitis is a form of chronic prostatitis, accompanied by the formation of stones (prostatoliths). Cumulative prostatitis is the most common complication of a long-term inflammatory process in the prostate gland, which must be dealt with by specialists in the field of urology and andrology. During the preventive ultrasound examination, prostate stones are detected in 8. 4% of men of various ages. The first age peak in the incidence of passive prostatitis occurs at the age of 30-39 and is due to an increase in cases of chronic prostatitis caused by STDs (chlamydia, trichomoniasis, gonorrhea, ureaplasmosis, mycoplasmosis, etc. ). In men aged 40-59 years, asphyxiant prostatitis, as a rule, develops in the context of prostate adenoma, and in patients over 60 years of age it is associated with a decrease in sexual function.

Causes of cumulative prostatitis
Depending on the cause of formation, prostate stones can be true (primary) or false (secondary). Primary stones initially form directly in the alveoli and ducts of the gland, secondary stones migrate to the prostate from the upper urinary tract (kidneys, bladder or urethra) if the patient has urolithiasis.
The development of prostatitis stone is caused by congestive and inflammatory changes in the prostate gland. Impaired emptying of the prostate glands is caused by BPH, irregular or lack of sexual activity and sedentary lifestyle. In this context, the addition of a dormant genitourinary tract infection leads to obstruction of the prostatic ducts and a change in the nature of the prostatic secretion. In turn, prostate stones also support a chronic inflammatory process and stagnation of secretions in the prostate.
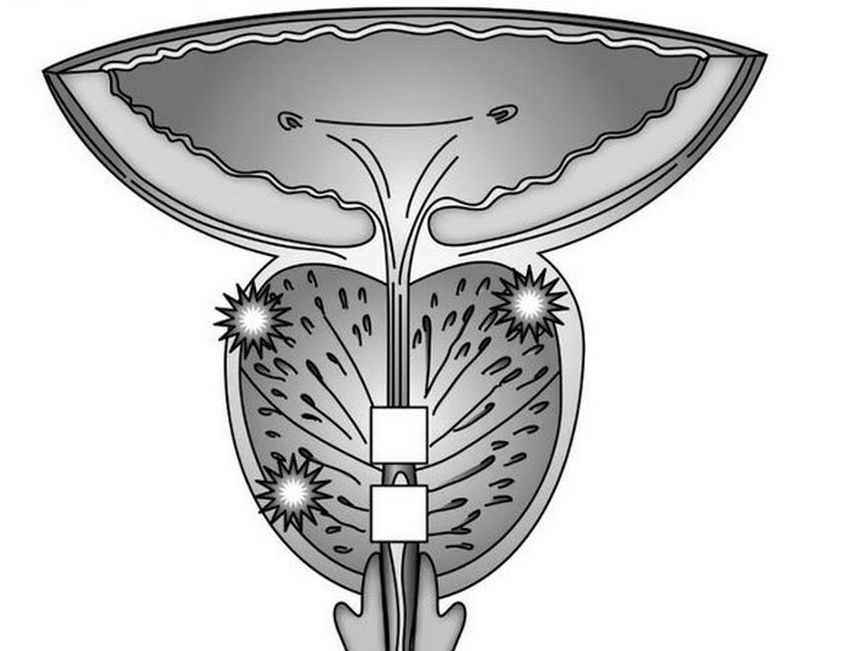
In addition to stagnation and inflammatory phenomena, urethro-prostatic reflux plays an important role in the development of pathological prostatitis - the pathological reflux of a small amount of urine from the urethra into the ducts of the prostate during urination. At the same time, the salts contained in the urine crystallize, thicken and over time turn into stones. The causes of urethro-prostatic reflux may be urethral strictures, trauma to the urethra, atony of the prostate and testicular tubercle, previous transurethral resection of the prostate, etc.
The morphological core for prostate stones are amyloid bodies and desquamated epithelium, which gradually become "overgrown" with phosphates and calcium salts. Prostate stones are located in cystically distended cells (lobes) or in the excretory ducts. Prostatoliths are yellowish in color, spherical in shape and vary in size (on average from 2. 5 to 4 mm). it can be single or multiple. In terms of their chemical composition, prostate stones are identical to bladder stones. With cumulative prostatitis, oxalate, phosphate and urate stones are formed more often.
Prostatitis suffocation symptoms
The clinical manifestations of calculous prostatitis generally resemble the course of chronic inflammation of the prostate. The main symptom in the clinic of prostatitis suffocation is pain. The pain is dull, pain in nature. located on the perineum, scrotum, above the pubic bone, sacrum or coccyx. Exacerbation of painful attacks may be associated with defecation, sexual intercourse, physical activity, prolonged sitting on a hard surface, prolonged walking, or erratic driving. Cumulative prostatitis is accompanied by frequent, sometimes complete urinary retention. haematuria, prostatorrhea (leakage of prostate secretions), haemospermia. It is characterized by decreased libido, weak erection, impaired ejaculation and painful ejaculation.
Endogenous prostate stones can remain in the prostate gland for a long time without symptoms. However, a long course of chronic inflammation and associated prostatitis stone can lead to the formation of prostatic abscess, the development of cystitis, atrophy and hardening of the glandular tissue.
Diagnosis of cumulative prostatitis
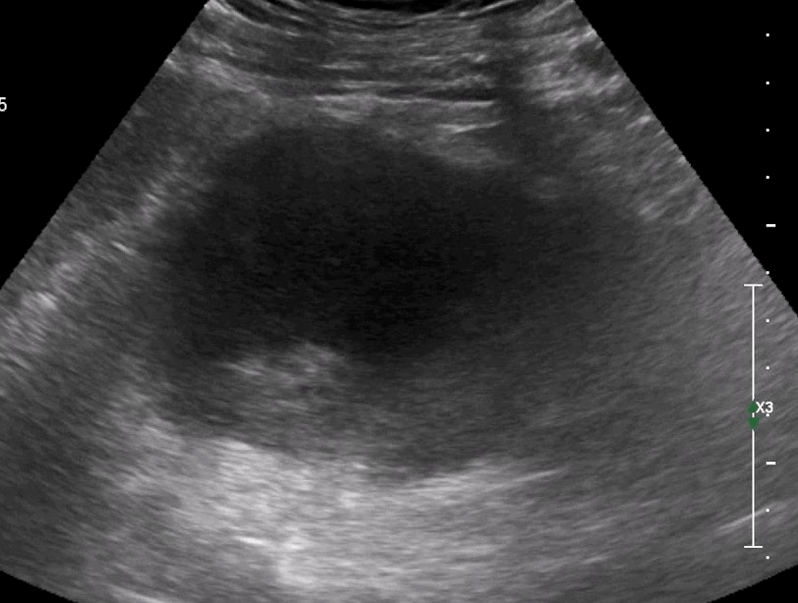
To establish the diagnosis of passive prostatitis, a consultation with a urologist (andrologist), an evaluation of the existing complaints and a physical and instrumental examination of the patient is required. When conducting a digital rectal examination of the prostate, the bulky surface of the stones and a kind of erythema are determined by palpation. Using transrectal ultrasound of the prostate gland, stones are detected in the form of ultrasound formations with a clear acoustic path. their location, quantity, size and structure are specified. Sometimes urography, CT and MRI of the prostate are used to detect prostatitis. Exogenous stones are diagnosed by pyelography, cystography and urethrography.
The instrumental examination of a patient with a prostatitis stone is supplemented by laboratory diagnosis: examination of prostate secretions, bacteriological culture of secretions and urine from the urethra, scraping PCR examination for sexually transmitted infections, biochemical analysis of blood and urine, determination of the level of the prostate. -specific antigen, sperm biochemistry, ejaculate culture, etc.
When conducting an examination, suffocating prostatitis is differentiated from prostate adenoma, tuberculosis and prostate cancer, chronic bacterial and bacterial prostatitis. In passive prostatitis not associated with a prostatic adenoma, the prostate gland volume and PSA level remain normal.
Treatment of prostatitis asphyxiation

Uncomplicated stones in combination with chronic inflammation of the prostate gland require conservative anti-inflammatory treatment. Treatment of prostatitis stone includes antibiotic therapy, non-steroidal anti-inflammatory drugs, herbal therapy, physical therapy procedures (magnetic therapy, ultrasound therapy, electrophoresis). In recent years, low-intensity laser has been successfully used for the non-invasive destruction of prostate stones. Prostate massage for patients with suffocating prostatitis is strictly contraindicated.
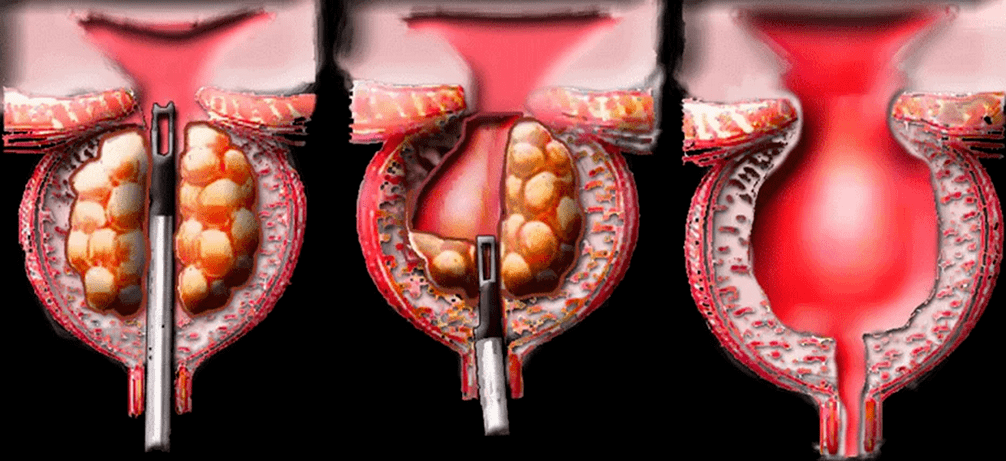
Surgical treatment of prostatitis stone is usually required in case of a complicated course of the disease, combining it with prostate adenoma. When a prostate abscess forms, the abscess opens and together with the discharge of pus, the passage of stones is also noted. Sometimes mobile extraneous stones can be pushed with instruments into the bladder and lithotripsy. Removal of large fixed stones is performed during the perineal or suprapubic incision procedure. When passive prostatitis is combined with BPH, the optimal method of surgical treatment is adenosectomy, TUR of the prostate, prostatectomy.
Treatment of prostatitis asphyxiation
Cumulative prostatitis is an inflammation of the prostate gland, complicated by the formation of stones. This type of prostatitis is a consequence of long-term chronic inflammation of the prostate. The disease is accompanied by frequent urination, annoying pain in the lower abdomen and perineum, erectile dysfunction and the presence of blood inclusions in the ejaculation.
Causes of this disease
Calculous is a form of chronic prostatitis characterized by stone formation. The disease is often a complication of a long-term inflammatory process in the prostate. In the context of chronic inflammation under the influence of negative internal and external factors, the secretion stagnates, which over time crystallizes and turns into stones.
In addition to congestion and inflammatory phenomena, urethro-prostatic reflux, characterized by the pathological reflux of a small amount of urine from the urethra into the ducts of the prostate gland during urination, plays an important role in the development of pathological prostatitis. The salts contained in the urine gradually crystallize and over time turn into dense stones. Common causes of uroprostatic reflux:
- urethral injuries;
- atony of the prostate and testicular tubercle;
- previous surgeries and invasive procedures.
Other pathologies that increase the risk of prostate stone formation:
- varicose veins of the small pelvis;
- metabolic disorders due to systemic pathologies.
Factors contributing to the development of pathological prostatitis:
- an inactive lifestyle that contributes to the development of stagnant processes in the pelvic organs.
- irregular sex life;
- alcohol abuse, smoking;
- uncontrolled use of certain groups of drugs.
- damage to the prostate during surgical procedures, long-term catheterization.
Types of stones in cumulative prostatitis
Depending on the number of stones, there are single and multiple. Depending on the underlying causes, prostate stones are:
- True. They are formed directly in the sinuses and ducts of the gland.
- False. They migrate to the prostate from the upper urinary tract: kidneys, bladder, urethra.
Stone formation in the prostate gland is identical in composition to bladder stones. With suffocating prostatitis, the following types of stones are most often formed:
Symptoms of the disease
The symptoms of prostatitis suffocation resemble the course of a chronic inflammatory process. The main symptom in the clinical picture of the disease is pain, the nature of which can be aching and dull. Location of pain: sacrum or coccyx.
A painful attack worsens during defecation, sexual intercourse, physical activity, prolonged sitting on a hard surface and prolonged walking.
Other symptoms of pathology:
- Frequent urination or complete retention of urine.
- hematuria and presence of blood inclusions in ejaculation.
- prostatorrhea – leakage of prostate secretions.
- decreased libido, erectile dysfunction, painful ejaculation.
- neurological disorders: irritability, increased fatigue, insomnia.
If you have any of the above symptoms, you should make an appointment with a urologist as soon as possible. The lack of adequate treatment and the long course of chronic passive prostatitis is fraught with serious, sometimes life-threatening consequences:
- atrophy and hardening of glandular tissues.
- prostate abscess.
Diagnostics
To make an accurate diagnosis, a consultation with a urologist-andrologist is necessary. During the initial examination, the specialist carefully listens to the patient's complaints, collects memories and asks additional questions that will help determine the causes of prostatitis and risk factors.
The doctor then performs a rectal examination of the prostate, which involves palpating the gland through the rectum. The technique allows you to assess the size, shape, structure of the gland, detect stones, determine the inflammatory process by increasing the size and pain during pressure. To confirm the diagnosis, additional laboratory and instrumental methods are prescribed.
Laboratory diagnosis
A number of additional laboratory tests used to diagnose asphyxiant prostatitis:
- Culture of prostate secretions. An important informative method for identifying pathogenic microorganisms and diagnosing the inflammatory process in the prostate gland.
- Urine culture. It allows you to detect a pathogenic infection in the urine, as well as determine its type and concentration. A culture is performed to clarify the diagnosis if inflammation of the prostate gland is suspected.
- PCR study of scrapings. It allows you to detect sexually transmitted infections and determine the pathogen.
- PSA analysis. It allows you to rule out prostate cancer, which often occurs in the context of prostatitis.
- General clinical analysis of blood and urine. It is prescribed to identify hidden inflammatory processes in the urinary system and kidney disorders.
- Spermogram. Ejaculation analysis to rule out or confirm infertility.
Instrumental diagnosis
Instrumental methods used to diagnose the pathology:
Prostate ultrasound. It allows you to detect stones, clarify their location, quantity, size, structure. Ultrasound will also help differentiate inflammation of the prostate from other diseases accompanied by similar symptoms.
Research urography. A contrast-enhanced X-ray method that makes it possible to detect prostate stones, their size and location.
CT or MRI of the prostate. It allows layer-by-layer scanning of the prostate gland and surrounding tissues. Using CT or MRI images, the doctor can study the structure of the prostate in detail, identify pathological foci, evaluate their location, size and relationship with the surrounding tissues.
Treatment of prostatitis asphyxiation
If the disease is not a complication and the general condition of the patient is satisfactory, the treatment of prostatitis stone is carried out on an outpatient basis. If the disease is accompanied by complications, in combination with an adenoma of the prostate, hospitalization of the patient is required.
Conservative therapy
The main goals of conservative treatment are the elimination of pathological symptoms. For this, the patient is prescribed a course of drug therapy, which includes the use of the following groups of drugs:
- Antibiotics. Destroy the infection, stop the inflammation. The type of drug, the dosage and the duration of the course for each patient are determined individually.
- Non-steroidal anti-inflammatory drugs. They stop the inflammatory process and help eliminate pathological symptoms: pain, swelling.
- Anticonvulsants. Relieves muscle spasms and relieves pain.
- Alpha adrenergic blockers. Facilitate the process of urination.
- Vitamin-mineral complexes, immunomodulators. Strengthen the immune system and promote rapid recovery.
As a supplement to complex drug therapy, doctors often prescribe physical therapy procedures that allow:
- elimination of stagnant processes.
- activates tissue regeneration.
- The most effective physiotherapy methods for suffocating prostatitis:
- ultrasound therapy, shock wave therapy.
Effective treatment of prostatitis suffocation is ensured by lifestyle changes. To prevent relapses, it is recommended to include physical activity, especially if your job requires you to be sedentary. Moderate physical activity improves blood circulation in the pelvic organs, eliminates congestion and strengthens local immunity.
Surgery
Surgical treatment is performed in case of complicated course of the disease and combination with prostatic hyperplasia. When an abscess forms, the surgeon opens the abscess. Along with the discharge of pus, the passage of stones is often observed. Large fixed stones are removed during a perineal or suprapubic incision. When passive prostatitis is combined with benign prostatic hyperplasia, the optimal methods of surgical treatment are transurethral resection of the prostate.
Chronic suffocating prostatitis
The term hard prostatitis defines the pathology of the prostate gland, in which stones form in its tubules. This disease is characterized by weakened penile erection and pain in the groin.
Causes and mechanism of development of suffocative prostatitis
A prolonged inflammatory process or congestion in the prostate ducts leads to the accumulation of secretions and mucus in them. Bacteria settle in these accumulations and calcium salts precipitate. The mucus thickens over time and turns into small stones that look like sand. They stick together and form pebbles.
There are several predisposing factors for the development of suffocative prostatitis:
- Chronic sexually transmitted infections (STDs)
- prolonged course of the infectious process with inflammation of the prostate ducts and tissues.
- congestion in the prostate, which is mainly related to a man's irregular sex life.
- urethro-prostatic reflux - pathological reflux of a small volume of urine into the prostate.
- genetic predisposition – presence of relatives with asphyxiant prostatitis.
Knowledge of the causes of the development of stones in the prostate gland is necessary for high-quality and adequate etiological treatment, which helps to prevent the recurrence of prostatitis stones.
Prostatitis suffocation symptoms
Cumulative prostatitis symptoms develop over a long period of time and a man may not pay attention to them. The clinical picture of the disease may include symptoms such as dull pain in the lower abdomen and waist, sacrum, perineum and pubic abdomen.
The pain may begin or intensify after defecation, sexual intercourse, vigorous physical activity, and other triggers. Dysuric disorders are observed - frequent urge to go to the toilet, painful or difficult urination, burning in the urethra and lower abdomen, and sometimes urinary retention occurs due to obstructions in the form of stones.
Patients experience prostatorrhea - involuntary discharge of the prostate during rest or during physical activity, straining during bowel movements or urination. There may be blood in the urine and semen.
Almost always, against the background of persistent inflammation with the formation of stones, sexual dysfunctions develop - weakened erection, premature ejaculation, decreased libido.
The main signs of suffocative prostatitis include:
- erectile dysfunction?
- pain in the groin, which can be throbbing and paroxysmal.
- during ejaculation - indicates damage to the vessels of the prostate tubules from the sharp edges of the stones.
- premature and painful ejaculation.

Such symptoms lead to a decrease in sexual desire.
Often men attribute it to the age factor, mistakenly believing that such sexual dysfunctions will not disappear. Sometimes they begin to self-medicate using various erectile stimulants (PDE-5 inhibitors).

This approach is very dangerous, as it can worsen the course of the pathological process and lead to the development of complications.
Prostatitis is an inflammatory pathological process in the prostate gland of a man. In most cases it is caused by an infection, which gradually leads to a chronic, long-term course of the disease and the development of complications.
Treatment of prostatitis stone is complex
- antibiotics,
- anti-inflammatory drugs,
- enzymes
- immunological drugs
- herbal medicine,
- physical therapy procedures.

Antibacterial agentsprescribed as part of etiotropic therapy. Their intake is necessary to suppress the activity of the causative agent of the infectious-inflammatory process. This can be both non-specific microbial flora (streptococci, staphylococci, enterococci, Escherichia coli, Proteus) and specific pathogens of urogenital infections - gonococci, chlamydia, ureaplasma, trichomonads, etc.
The choice of antibiotics can be based on the results of a culture study of prostate secretions and the determination of the sensitivity of the microbial pathogen to the drugs. Antibiotics are sometimes prescribed empirically based on scientifically proven antimicrobial efficacy of the drugs. The choice of antibiotics, the determination of the dose and the duration of their use can be made exclusively by the attending physician, as their uncontrolled use can lead to serious complications and worsen the course of the underlying disease.
If the tissues of the prostate gland are parasitized by multi-related microbial flora (bacterial, viral microorganisms, protozoa), the etiotropic treatment regimen will consist of a complex of different drugs that act in a certain antimicrobial spectrum.
To stimulate the body's immune defensesand its resistance to infections, immunomodulatory drugs are prescribed - Immunomax, Panavir, Interferon and its derivatives. To improve the antimicrobial effect of etiotropic drugs, enzymatic agents are prescribed with them - longidase, chemotrypsin. They facilitate the administration of active antibiotic substances to the affected tissues, have an indirect analgesic effect and have an anti-inflammatory and regenerative effect.
The pain syndrome is relieved withuse of non-steroidal anti-inflammatory drugs. Along with antibiotic treatment, probiotics are prescribed to prevent the development of intestinal dysbiosis. In order to protect the liver parenchyma from the toxic effects of antibacterial drugs and to improve its functional state, hepatoprotectors are prescribed. After the subsidence of acute inflammatory phenomena, physiotherapeutic procedures are prescribed - laser therapy, magnetotherapy, mud therapy, galvanization, medicinal electrophoresis, reflexogenic therapy, material therapy, etc.
This improves metabolic processes, microcirculation, lymphatic drainage and tissue trophism of the prostate, stimulates the restoration of its functional state and helps to resolve inflammatory processes. A low frequency laser is used to destroy the stones. It crushes the stones and lets the small stones come out of the tubules. In case of complications in the form of prostate adenoma or abscess (restricted cavity filled with pus), surgery is performed.
It involves removing part of the prostate gland (resection). To avoid this, at the first signs of pathology, expressed in erectile dysfunction, you need to consult a doctor. Self-medication or ignoring the problem always leads to the subsequent development of complications.





























